Overview of Fundoplication Antireflux Surgery
The most common antireflux surgery is known as a fundoplication (fundo– means “top of stomach” and –plication means “to fold”). Fundoplication procedures involve surgeons wrapping the upper portion of the stomach around the end of the esophagus and stitching it in place. Surgeons use this technique to reinforce the antireflux barrier and the junction between the esophagus and the stomach. Surgeons have performed fundoplication surgery for over 50 years and it has proven successful at managing GERD symptoms.
By mechanically reconstructing the antireflux barrier, the technique aims to naturally reduce troublesome reflux by restoring the body’s normal defense.
Goals of Antireflux Surgery
The goal of a fundoplication is to treat the causes of GERD by restoring the normal functions of the junction between the esophagus and the stomach. Surgeons are able to accomplish this by wrapping the upper portion of the stomach (the fundus) around the esophagus either partially or totally. The specific goals of the surgery are:
- Reduction of a hiatal hernia (if present) by repairing the enlarged opening of the diaphragm and ensuring that the stomach and esophagus are properly positioned below the diaphragm
- Restoration of the angle at which the esophagus enters the stomach
- Increase in the pressure of the muscle that controls the valve between the stomach and the esophagus; this recreates a one-way valve to prevent reflux and control GERD
Types of Antireflux Fundoplication Surgery
Nissen Laparoscopic Surgery
Although fundoplication was first performed as open surgery, technological advances in the 1990s enabled a laparoscopic approach. A laparoscopic procedure involves surgeons accessing the abdomen via several small incisions. General anesthesia is required. The surgeon repairs any hiatal hernia before performing the fundoplication. Surgeons can perform laparoscopic fundoplication on patients with any size hiatal hernia. Patients typically return to work within 1-2 weeks.
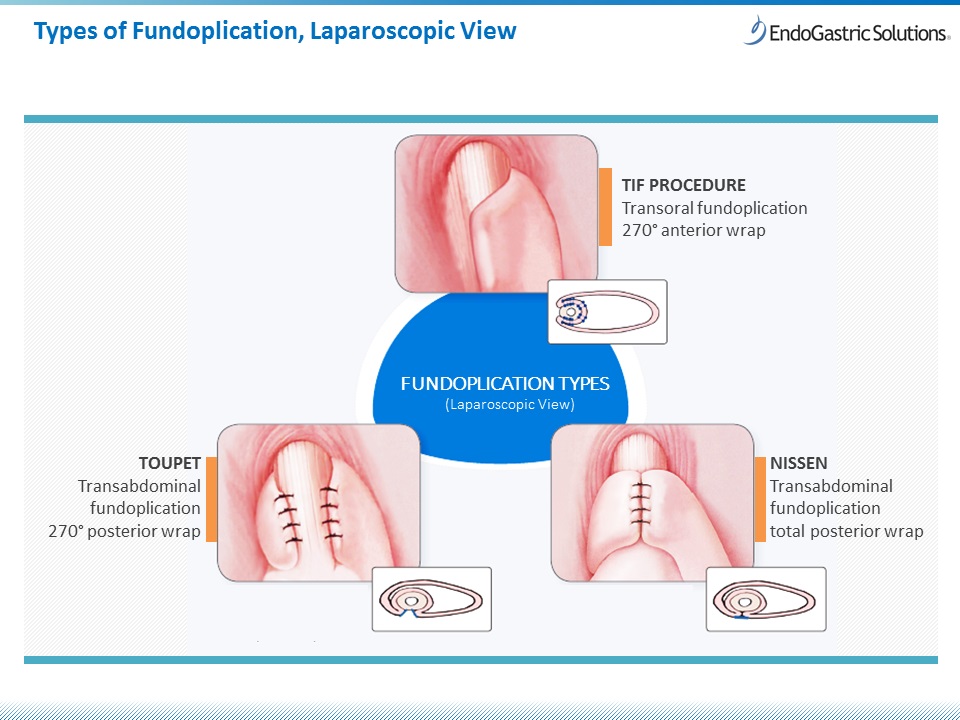
The so-called gold standard for antireflux surgery has been the laparoscopic Nissen procedure, a total fundoplication which wraps the fundus 360 degrees around the esophagus and results in a hyper functioning antireflux valve. Because the Nissen procedure modifies the esophagus and the stomach beyond normal anatomy, natural bodily functions such as belching and vomiting may be limited.
Some surgeons can also perform a partial fundoplication (i.e., a less than 360-degree wrap) which more closely mimics normal anatomy. However, this type of procedure can require more surgical precision and is not as common.
In a randomized study, 92% of patients who had laparoscopic Nissen fundoplications reported symptom control five years after the surgery.
However, it is important to remember that laparoscopic fundoplication is a traditional surgical procedure with inherent associated risks including bleeding, infection, and injury to internal organs. In order to wrap the fundus, surgeons need to cut away connective tissue in the abdomen (also known as dissection); this process creates scar tissue in the abdominal cavity making it a challenge to revise the procedure should the need arise.
Incisionless Surgery: The TIF Procedure
An incisionless approach is available for patients with smaller hiatal hernias. Since it is a fundoplication, the Transoral Incisionless Fundoplication (TIF) procedure treats the underlying cause of GERD. It has an excellent safety profile, with fewer side effects than conventional antireflux surgery. Surgeons perform the TIF procedure through the mouth with no abdominal incisions. Patients typically return to work in less than one week.
Associated complications are typically milder than for laparoscopic procedures, e.g. sore throat or difficulty swallowing. Any complications usually resolve within a few weeks of surgery. Since the procedure rebuilds the valve from within the stomach, there is no abdominal dissection and no abdominal scaring.
If GERD symptoms return after traditional antireflux surgery, the TIF procedure has been used to revise and rebuild the valve and vice versa.
The TIF procedure may also be performed immediately following a laparoscopic hiatal hernia repair when the hernia measures greater than 2 cm.
When to Consider Antireflux Surgery
Most people with mild GERD can successfully control symptoms through dietary and lifestyle changes. Sometimes people begin using over the counter and/or prescribed medicines. For patients who experience inadequate relief and/or side effects from medication, surgical intervention may be appropriate.
In addition, surgery may be suitable for patients who have any of the following:
- concerns about the long-term side effects or costs associated with medication
- certain complications of GERD (e.g. Barrett’s esophagus, narrowing of the inside space of the esophagus)
- atypical symptoms of GERD from regurgitation (e.g. asthma, hoarseness, cough, chest pain, aspiration)
Find a TIF-trained physician to discuss your treatment options.