How Physicians Diagnose GERD
As with all things medical, a doctor knows best: a diagnosis of GERD should always be made by your physician.
Physicians can often make diagnoses based on the presentation of common symptoms, especially in patients with more mild cases of GERD. However, more complicated GERD can be tricky to diagnose given the variability of symptoms and ways they may surface, requiring the trained eye of a medical professional to accurately spot the signs.
Tools Used to Diagnose GERD
There are a number of diagnostic tools a physician may use in the diagnosis of GERD, including these:
Endoscopy:
Doctors will perform an endoscopy procedure to examine the esophagus — the junction between the esophagus and the stomach — and the stomach for the presence of erosive esophagitis, as well as other potential concerns. The procedure involves physicians passing a flexible, lighted video scope (endoscope) through the mouth, down the esophagus, and into the stomach. You may also hear doctors call it esophagogastroduodenoscopy, or EGD; this type of procedure is normally quick and painless.
Upper GI Series:
An upper GI series (also known as barium swallow or esophagram) can help physicians spot anatomic abnormalities such as a hiatal hernia, blockages, inflammation of the esophagus, and free reflux. It is primarily used by doctors to rule out esophageal disorders such as achalasia, which can cause reflux-like symptoms. An upper GI series involves the patient ingesting a solution (barium) that can be seen via x-ray. The procedure typically takes about 30 minutes.
Manometry:
Manometry examines motility of the esophagus by assessing the strength and coordination of muscle contractions, as well as the relaxation and coordination of the upper and lower sphincter muscles of the esophagus. Manometry involves the physician passing a small tube through the nose into the esophagus. The test usually takes 30-45 minutes.
pH Monitoring:
pH monitoring provides a way for physicians to measure the severity of acid exposure in the esophagus. They can do the study using one of two methods:
- The first involves a physician inserting a small tube through the nose and placing it in the back of the patient’s throat for 24-48 hours.
- The second method involves a small electronic capsule. The physician will introduce this capsule through the patient’s mouth, attach it to the esophagus, and leave it in place for 48 hours. Most patients do not notice the capsule. The capsule will eventually fall off and pass on its own through the GI tract within a few days.
In both instances, patients are often asked to keep a diary to document when they eat, sleep, or experience symptoms.
Impedance:
Impedance involves the physician passing a small tube through the patient’s nose into the esophagus. The physician then leaves the tube in place for approximately 24 hours to measure how much reflux is occurring, whether or not the reflux is acidic, and how symptoms correlate with reflux.
Patient History Surveys:
Physicians have a number of surveys commonly used to understand patient symptoms and identify GERD. It is likely that your doctor will use one as part of a standard workup if he/she suspects GERD. One such test is the GERD-HRQL (GERD – Health Related Quality of Life) survey.
Prior to testing, you should discuss any inherent risks associated with the diagnostic procedures we have described here, or any others your physician suggests for the diagnosis of GERD. Also, consult your physician for more specific guidance on what to do before and after a procedure and what to expect during the procedure.
Having reflux from time to time is normal but having it interrupt your life is not. If you suffer symptoms of reflux twice or more per week, you may have GERD. Take the GERD-HRQL survey if you suspect a problem. Search for a TIF-trained physician to schedule a full GERD evaluation.
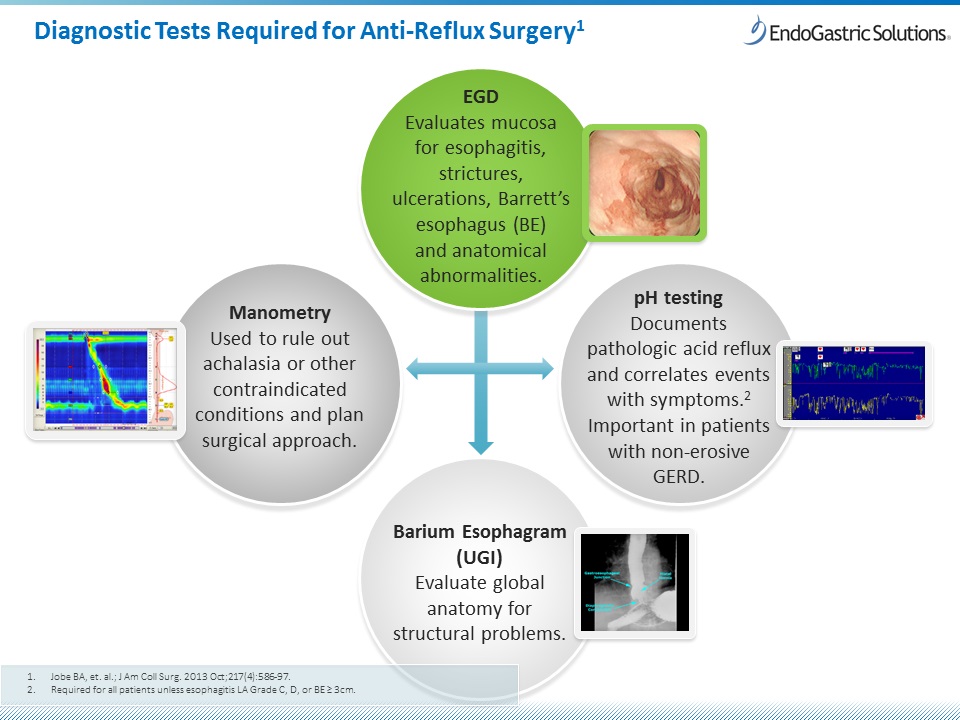
Picture above are four of the six methods physicians use for diagnosing GERD. These four tests help physicians determine if your case of GERD is severe enough to warrant anti-reflux surgery, such as the Transoral Incisionless Fundoplication (TIF) procedure.
NP02370-02B
NP02395-01J

