Published Clinical Results for the TIF Procedure
Clinical results to date for the TIF procedure have been comparable to traditional fundoplication procedures.(1)
When it comes to managing GERD (also known as gastroesophageal reflux disease) symptoms, the TIF procedure has excellent clinical results for patients.
The following clinical results data was generated from more than 100+ published studies which chronicle successful outcomes on over 1,500 unique patients with GERD symptoms from over 75 centers in the US and Europe. All published data consistently demonstrate:(2)
- Improved quality of life scores on a variety of questionnaires (validated instruments)
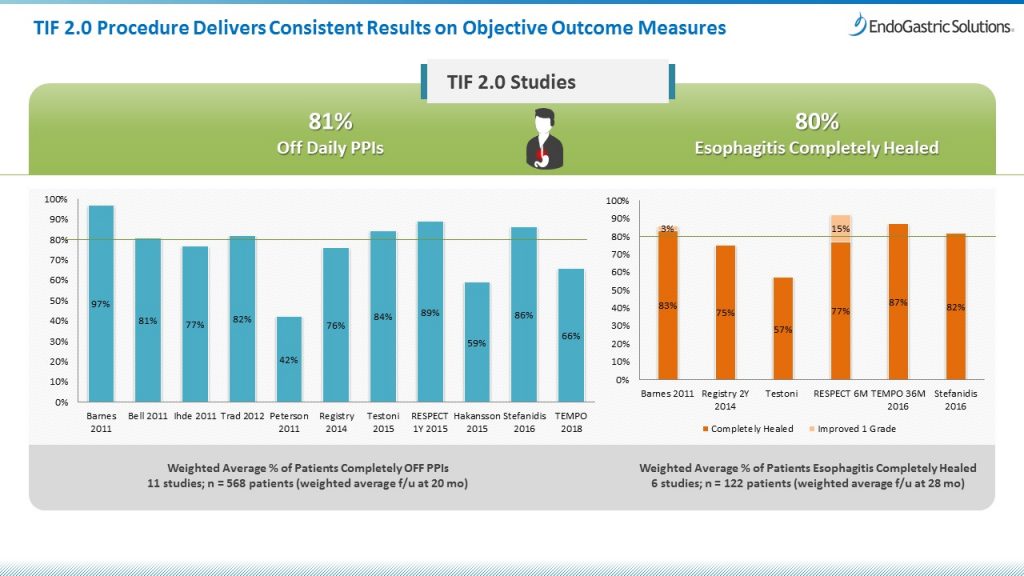
- Patients no longer dependent on daily PPI therapy (see charts below)
- Healing of esophagitis (see charts below)
- Improvements in acid exposure (pH parameters)
- The TIF procedure is very safe, with low rate of serious adverse events at less than 0.5%
- Virtual absence of long term side-effects associated with traditional fundoplication techniques
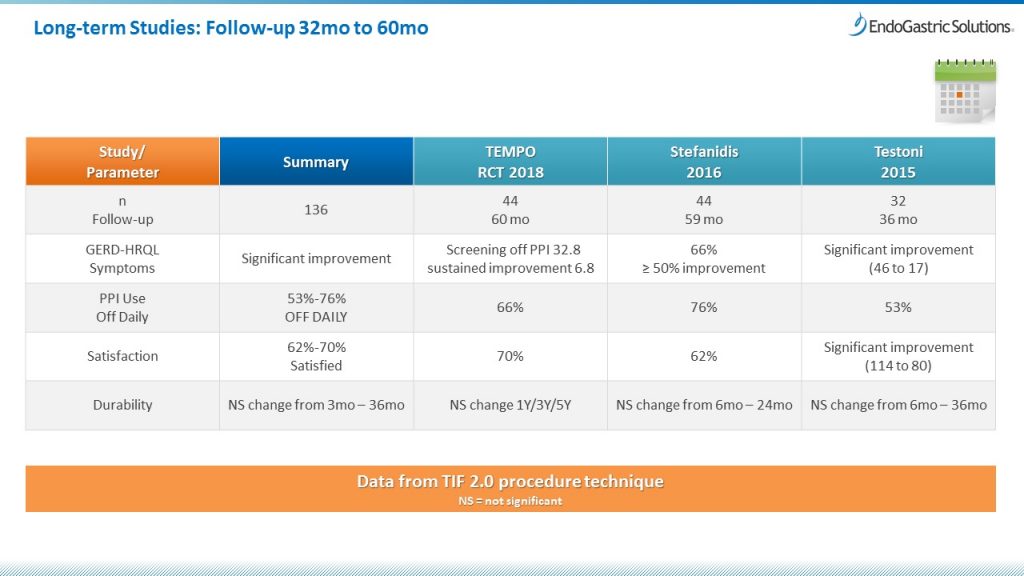
Long-term studies have followed patients for up to 5-years (see chart below) and include post-market registries and retrospective case series. Randomized controlled trials (RCTs) are the most academically rigorous study designs, and generate what’s known as Level I evidence. Two RCTs compared TIF patients with sham/placebo control groups–highly unusual for a medical procedure with a specific device.
Recent high-level clinical studies support the safety, effectiveness, and durability of the TIF procedure and justify its use as a therapeutic option to control typical and atypical symptoms of GERD, and where PPIs fail to achieve symptomatic control. The TIF procedure is now an established treatment alternative for appropriately selected patients with moderate to severe chronic GERD symptoms.
If you’d like to discuss the clinical results for the TIF procedure and learn what can be done to help your GERD, find a TIF-qualified physician near you.
Reference:
1. Toomey P, et al; Am Surg 2014 Sep;80(9):860-7.
2. Data on file at EGS.